Article: TSH Abnormalities and Treatment Algorithms in Primary Care
M3 India Newsdesk May 14, 2025
This article explains how to interpret and manage TSH abnormalities in primary care, with diagnostic strategies and treatment plans for subclinical and overt thyroid disorders.
Thyroid-stimulating hormone (TSH) plays a central role in regulating thyroid function and is frequently evaluated in primary care for symptoms such as fatigue, weight changes, and mood disturbances. Abnormalities in TSH can signal a range of thyroid disorders, from overt hypothyroidism to subclinical hyperthyroidism. Managing these conditions appropriately at the primary care level is crucial for preventing complications and ensuring optimal patient outcomes.
Understanding TSH and Thyroid Function Test
TSH is secreted by the anterior pituitary and regulates the production of T3 and T4 from the thyroid gland. Its levels are inversely proportional to thyroid hormone levels due to a negative feedback mechanism.
Thyroid function tests are not done in:
- Sick-ICU patients
- On fasting
- Chronic systemic illness
- Higher iodide levels
(In all these circumstances, Type 2 deiodinase is inhibited, and large amounts of Type 3 will be produced. Conversion of T4 to T3 is inhibited and will result in the formation of rt3

Hyperthyroxinemia: When T3 and T4 are both increased,
Thyrotoxicosis. → Free T3-T4 increases
If total T3-T4 increases but free T3-T4 is normal, Euthyroid (normal) state → Euthyroid hyperthyroxinemia → Thyroid Binding Globulin Excess (main reason).
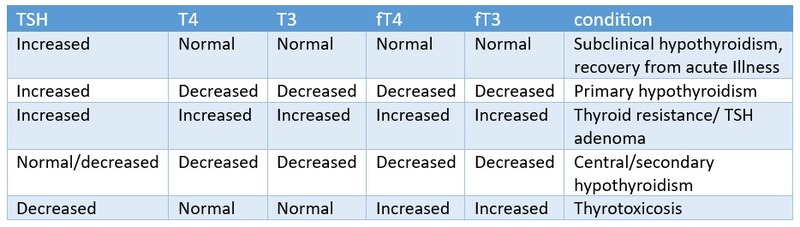
Interpretation
- Normal TSH: 0.4–4.0 mIU/L (may vary slightly by laboratory)
- Elevated TSH with low fT4/fT3: Overt/ primary hypothyroidism
- Elevated TSH with normal fT4/fT3: Subclinical hypothyroidism
- Elevated TSH with high fT4/fT3 – TSH secreting adenoma of pituitary
- Low TSH with high fT4/fT3: Overt / primary hyperthyroidism/ thyrotoxicosis
- Low TSH with normal fT4/fT3: Subclinical hyperthyroidism
- Low TSH with low fT4/fT3: - central (secondary) hypothyroidism, sick euthyroid
Causes of TSH Abnormalities
1. Elevated TSH
- Hashimoto’s thyroiditis
- iodine deficiency
- post-thyroidectomy or radioiodine therapy
- medications (e.g., lithium, amiodarone)
2. Low TSH
- Graves’ disease
- toxic multinodular goitre
- thyroiditis
- exogenous thyroid hormone intake
Approach to Evaluation
- Confirm abnormal TSH: Repeat testing, especially in subclinical states
- Assess free T4 (and T3 if needed)
- Evaluate for symptoms and signs
- Check for thyroid antibodies (e.g., anti-TPO) if hypothyroidism is suspected
- Ultrasound or radionuclide scan in suspected hyperthyroid states
Treatment Algorithms
1. Subclinical Hypothyroidism (TSH 4.5-10 mIU/L, normal free T4)
Treat if:
- TSH >10 mIU/L
- Positive anti-TPO antibodies
- Pregnant or planning pregnancy
- Symptomatic patient
Start Levothyroxine at 25-50 mcg/day
Monitor TSH every 6-8 weeks, then 6-monthly once stable
2. Primary Hypothyroidism (TSH >4 mIU/L, low fT4)
- Initiate Levothyroxine at full replacement dose (1.6 mcg/kg/day in adults)
- Lower dose in elderly or cardiac patients (25-50 mcg/day)
- Monitor TSH every 6-8 weeks
L-thyroxine on empty stomach 1.6-1.8 mcg/kg/day at 7 am (ideal time as per studies) → 30 mins later, can take a meal.
Increased requirement seen with-
- Drugs which increase the metabolism: Carbamazepine, Rifampicin, oestrogen & phenytoin.
- Drugs which decrease absorption: iron sulphate, Ca, Al(OH)3, Cholestyramine
- Pregnancy.
- GI disorders.
Target TSH – lower normal range
3. Secondary Hypothyroidism (TSH low/lower normal, low fT4)
Lower dose 25-50 mcg/day
4. Subclinical Hyperthyroidism (TSH <0.4 mIU/L, normal T3/T4)
- Observe if TSH >0.1 mIU/L and asymptomatic
- Treat if TSH <0.1 mIU/L, especially if:
- Age >65 years
- Cardiovascular disease or osteoporosis
- Symptomatic
- Beta blockers for symptom control
5. Primary hyperthyroidism (TSH undetectable, high T3/T4)
Antithyroid drugs (e.g., Methimazole)
Beta blockers for symptom relief
Refer to an endocrinologist for radioiodine therapy or surgery if needed
Management of Graves' Disease
Radioiodine is the definitive treatment. In 1/3 to 1/2 of patients (30-60%), permanent remission was achieved with antithyroid drugs.
Drugs given for 18 months (up to 24 months sometimes).
Antithyroid Drugs:
1. Thionamides
6mg methimazole = 10 mg carbimazole = 100 mg Propylthiouracil (PTU).
2. PTU
- PTU is the drug of choice in pregnancy (due to more plasma protein binding).
- In pregnancy, only during 1st trimester, then changed to methimazole/carbimazole (practically).
- Propylthiouracil is hepatotoxic.
3. Methimazole
- The half-life of methimazole is 6 hrs.
- It is an irreversible inhibitor.
- Usually started at 3 mg TDS.
- Produces aplasia cutis/choanal atresia.
4. Carbimazole
- Half-life: 8 hours
- Started as 5 mg TDS
Dose titration is done at 4-6 weeks, depending on fT3, FT4 levels.
30 to 60% (1/3) achieve remission in 12 to 18 months.
The commonest side effect is rash most dangerous side effect is agranulocytosis (0.2%), and is dose-related; monitor for WBC count
PTU can cause:
- Cholestasis
- Hepatitis
- Drug-induced lupus
- Anca vasculitis
- Hirata's disease. Anti-Insulin Antibody-related syndrome- Hypoglycemia
Case Study 1
Subclinical Hypothyroidism in a Middle-Aged Woman
Mrs. D, a 48-year-old female, presents with fatigue and mild weight gain. TSH is 6.8 mIU/L, free T4 is normal. She has positive anti-TPO antibodies.
Diagnosis: Subclinical hypothyroidism
Management: Started on Levothyroxine 25 mcg/day. TSH normalised in 8 weeks. Symptoms improved.
Case Study 2
Primary Hyperthyroidism in a Young Male
Mr. K, a 32-year-old male, presents with palpitations, anxiety, and weight loss. TSH is <0.01 mIU/L, T3 and T4 elevated. Thyroid scan confirms Graves' disease.
Management: Started on Methimazole and propranolol. Referred for endocrinology follow-up. Euthyroid state achieved in 3 months.
Conclusion
TSH abnormalities are common and manageable in the primary care setting with a structured approach. Distinguishing between subclinical and overt disease is essential for appropriate treatment decisions. Regular monitoring and patient education are key to successful management.
Disclaimer: The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Khemeswar Agasti is an MD in General Medicine from Cuttack.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries