Article on The Global Threat of Antibiotic Resistance
M3 India Newsdesk May 21, 2025
In the 21st century, Antibiotic Resistance (AR) has become one of the biggest risks to world health. The causes, spread, and mechanism of action of AR are elucidated in this article. This article also presents 2 case studies related to AR.
Introduction
Antibiotic Resistance AR is one of the top ten worldwide public health threats, according to the World Health Organisation (WHO) [1]. With bacteria increasingly outsmarting our pharmaceutical defences, we are edging closer to a post-antibiotic era, where minor infections could once again become fatal.
Causes and Spread of Resistance
The misuse and overuse of antibiotics in humans, livestock, and agriculture are primary drivers. Inappropriate prescriptions, incomplete courses of treatment, and unsupervised antibiotic use in low-income countries further aggravate the situation [2]. Global travel and trade also facilitate the transcontinental spread of resistant strains.
Mechanisms of Resistance
Bacteria develop resistance through various mechanisms: enzymatic degradation of drugs, alteration of drug targets, efflux pumps expelling antibiotics, and reduced permeability. These changes may arise from spontaneous mutations or horizontal gene transfer [3].
Case Study 1: NTM infection: A Myth!!!
A 27-year-old patient was started on anti-tubercular therapy based on a positive Sputum AFB (Grade 3+), despite GeneXpert being negative for M. tuberculosis. An AFB culture was advised due to suspected NTM but was delayed for months, during which the patient deteriorated. When finally performed, culture revealed Mycobacterium abscessus. Delayed diagnosis and inappropriate therapy led to antimicrobial resistance and clinical worsening. This case underscores the need for timely lab-clinician communication and strict adherence to diagnostic protocols.
Impact on Health and Economy
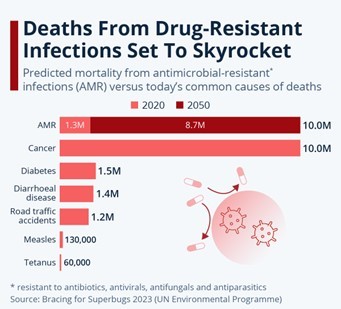
AR leads to prolonged hospital stays, increased medical costs, and heightened mortality. According to the OECD, resistant infections cause approximately 700,000 deaths globally each year—a number projected to rise to 10 million by 2050 if unchecked [4]. Economically, AR could cost the world over $100 trillion in lost productivity.
Projected Deaths Due to AMR by 2050
Global Response and Challenges
International efforts include the WHO’s Global Action Plan – Global AMR Surveillance System (GLASS) and national strategies like India’s National Action Plan on AMR (NAP-AMR), 2017. However, challenges remain: underfunded health systems, lack of diagnostics, and insufficient new antibiotics in the pipeline [5].
Case Study 2: Carbapenem-Resistant E. coli (CRE) in a Community Setting
A 64-year-old woman in a tier-II city presents with recurrent urinary tract infections. Cultures reveal Carbapenem-resistant E. coli, resistant to most drugs, even fosfomycin and nitrofurantoin, commonly used in UTIS. Community-acquired infections like this are becoming more common, complicating outpatient treatments and burdening healthcare systems.
However, with the availability of detection of carbapenemase resistant marker genes – KPC, NDM, IPM, VIM and OXA-48, nowadays newer targeted agents such as Ceftazidime-Avibactam ± Aztreonam, Cefepime-Zidebactam, Meropenem-Vaborbactam, Meropenem-nacubactam, Imipenem-relebactam, Tigecycline, Plazomicin, or Cefiderocol can be used as targeted therapy.
Role of Healthcare Professionals
Clinicians, microbiologists, and pharmacists play a pivotal role in antibiotic stewardship. Rational prescribing, use of rapid diagnostics, and continuous education can curb unnecessary antibiotic usage. Campaigns to raise public awareness are equally important [8].
Conclusion
Antibiotic resistance is a complex and evolving crisis that requires a coordinated, global response. Through effective policies, education, and innovation, it is possible to preserve the efficacy of antibiotics for future generations. The time to act is now.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Anirudh Gupta is a Senior Consultant Microbiologist from New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries
