Article on Monitoring Nutritional Status in Hospitalised Patients: A Physician’s Guide
M3 India Newsdesk Jun 23, 2025
This article highlights the hidden burden of malnutrition in Indian hospitals and its impact on recovery. It offers practical strategies for physicians to detect, monitor, and manage nutrition as part of routine clinical care.

Malnutrition remains a silent yet serious issue in hospitals throughout India. It doesn’t always present as underweight; it might be concealed by oedema, chronic illness, or even a normal BMI. Nutrition often gets overlooked amidst the rush of rounds, investigations, and clinical decisions. But as physicians, what if we viewed food as medicine too? This guide provides practical, evidence-based strategies to monitor and support nutritional status in hospitalised patients, particularly in Indian clinical contexts.
Why Monitoring Nutrition is a Clinical Priority
Data from Indian studies show that up to 40–50% of hospitalised patients are either malnourished or at high risk. Poor nutrition doesn’t just affect recovery—it affects survival. Malnutrition leads to:
- Longer hospital stays
- Higher infection risk
- Impaired wound healing and delayed recovery
- Increased need for antibiotics and other interventions
- Higher readmission and mortality rates
Nutrition should be seen not just as support, but as therapy.
Clinical Signs Physicians Should Watch For
You don’t always need a screening tool to suspect malnutrition. Simple observation and history-taking can reveal a lot. Look for:
- Noticeable weight loss in the last 3–6 months
- Loss of muscle over temples, shoulders, and clavicles
- Low appetite, skipping meals, NPO status >2 days
- Gastrointestinal issues (diarrhoea, nausea, bloating)
- Fluid overload that may be masking weight loss
- Chronic conditions with catabolic states (cancer, CKD, sepsis)
Ask simple questions like:
- “How’s your appetite been in the past week?”
- “Have you lost any weight recently—intentionally or unintentionally?”
Screening Tools to Use in Indian Hospitals
For quick but structured screening, use:
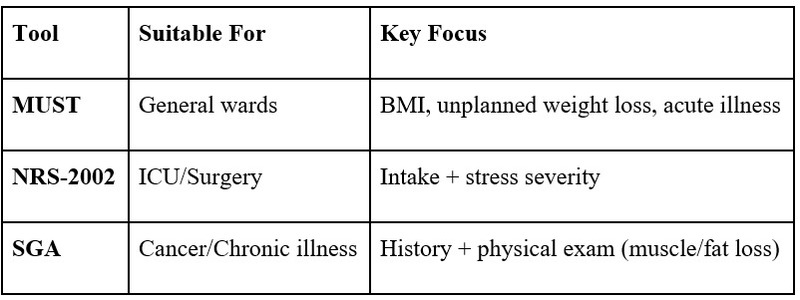
Many Indian hospitals now integrate these tools into EMRs or nursing protocols. Physicians should ensure a tool is used within 24–48 hours of admission and reassessed every 5–7 days.
Labs: Supportive but Not Diagnostic
Interpret nutritional labs carefully. Inflammation or infection can alter results.
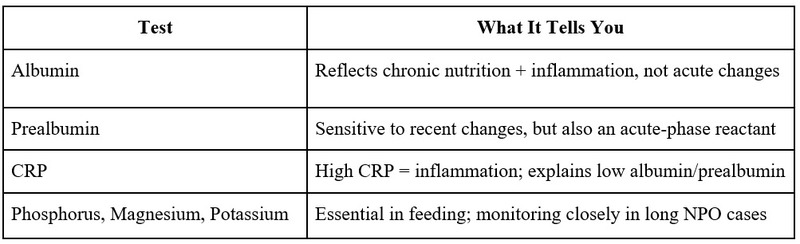
In Indian ICUs, it’s common to see low magnesium or phosphorus in septic or diabetic patients—this increases the risk of arrhythmia or refeeding syndrome.
Build a Strong Physician-Dietitian Partnership
In many Indian settings, physicians still make all care decisions. But effective nutrition care requires teamwork.
What doctors can do:
- Refer to the dietitian early—don’t wait for obvious signs
- Share diagnosis, prognosis, fluid restrictions, and goals
- Avoid unnecessary NPO orders unless clinically justified
- Opt for enteral nutrition unless there’s a strong contraindication
Daily ward rounds should include a basic nutrition review: intake, tolerance, and dietitian input. In Indian hospitals, this is improving, but it is still inconsistent.
Tailored Approaches for Vulnerable Groups
- Elderly: Watch out for sarcopenia. Encourage soft, protein-rich foods like paneer, pulses, egg whites, or protein-enriched liquids.
- ICU Patients: Start feeds within 24–48 hours. Calculate energy needs based on ideal body weight or use indirect calorimetry if available.
- Post-Surgical Patients: Don’t delay feeding unnecessarily. Clear liquids can be started as soon as bowel sounds return.
- Cancer Patients: Early enteral feeding can counteract cachexia. Use nutrient-dense, easily digestible small meals.
What to Monitor Daily
- Intake-output charts (actual consumption, not just what’s offered)
- Body weight (2x/week minimum)
- GI symptoms (vomiting, diarrhoea, constipation)
- Blood sugar and electrolytes
- Signs of intolerance (distension, risk of aspiration)
- Functional recovery (mobility, alertness, strength)
Ask nursing staff: “Is the patient eating 75% of what’s given?” That alone can flag many risks.
Common Mistakes to Avoid
- Judging nutrition only by weight or BMI
- Assuming NPO for >24 hours is harmless
- Overusing parenteral nutrition without attempting oral or enteral
- Ignoring patient preferences, chewing/swallowing difficulties
- Not reassessing nutrition status during hospital stay
In the Indian context, diet diversity and cultural food preferences are critical. Many patients reject hospital food because it doesn’t match home flavors.
Quick Ward Round Nutrition Checklist
- Is the patient tolerating food or feed?
- Any recent weight or intake change?
- Are they on NPO or liquid-only for >24 hours?
- Have electrolytes, B12, and albumin been checked?
- Has the dietitian seen this patient?
Use this simple checklist to make nutrition part of clinical decision-making.
Conclusion: Make Nutrition a Bedside Habit
Nutrition care extends beyond food trays—it’s an essential part of the healing process. Physicians are trained to diagnose and prescribe, but let’s also prioritise nourishment. By incorporating simple screenings, close monitoring, and collaboration with dietitians, we can transform hospital malnutrition from an overlooked issue into a resolved one.
A patient who eats well heals well.
Case Studies
Case study 1: The overlooked malnutrition in a post-surgical patient
Patient Profile: Ms ABC, a 63-year-old female, was admitted post-cholecystectomy.
Clinical Timeline:
- Day 1–2: Kept NPO post-surgery without reassessment
- Day 3: Complained of weakness and nausea
- Lost 2 kg in 5 days.
- No nutrition referral was made until discharge was planned
Key Findings: BMI on admission: 21.5 (appeared “normal”)
Diet intake: <30% of meals over 4 days
Labs: Low serum albumin (2.8 g/dL), borderline magnesium
Intervention: Late referral to the dietitian on Day 5. Started on oral nutritional supplements + soft, high-protein Indian meals. Recovery delayed, discharge extended by 2 days.
Takeaway: Malnutrition was missed because she had “normal” weight. Earlier screening and proactive dietitian involvement could have prevented functional decline.
Case Study 2: ICU Patient with Hidden Risk of Refeeding Syndrome
Patient Profile: Mr PBK, a 48-year-old male with alcoholic liver disease, was admitted to the ICU with acute pancreatitis.
Clinical Timeline:
- Was NPO for 4 days due to vomiting
- Electrolytes: Phosphorus, potassium, and magnesium are low
- Feeding was initiated without micronutrient repletion
- Developed arrhythmia and required ICU stay extension
Intervention:
Refeeding syndrome suspected. Enteral feed paused, electrolytes corrected first. Restarted feeds with gradual advancement.
Takeaway:
Refeeding syndrome is underdiagnosed in Indian hospitals. Pre-checking electrolytes and slow feed advancement are critical.
Suggested Readings & Resources:
- ESPEN Guidelines on Clinical Nutrition
- Indian Dietetic Association Position Papers
- ASPEN Guidelines on Nutrition Support in Critically Ill
- Geriatric Nutrition Handbook (ICMR 2021)
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
The author of this article, Ms Rutambhara Nhawkar, is a Clinical Dietitian, M. Sc. (Clinical Nutrition & Dietetics), Certified Diabetes Educator and a medical writer from Pune.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries